Help
Out of network
When you go to a provider who is not in your network, you
may pay more for your care. You may also have to file your own claims.
Some plans do not provide any coverage for care received from
out-of-network providers, except under certain circumstances, including
but not limited to emergency and urgently needed services. Check your
coverage details or contact Humana for more information.
Your share
Your share is the amount you may owe your provider after your
plan benefits have been applied. Humana members with both Medicare and
Medicaid coverage may not be responsible for this amount and should
contact the provider for additional details.
Humana discounts
Humana has special rates with in-network providers that may
give you discounts on the amount you owe your provider. These are
savings to you and, are not included in the amount you pay.
Plan exclusion
A portion of your bill may be removed, or excluded, from the
total amount you owe. This is done based on the amount your provider is
allowed to charge for that benefit or service. Please check the reason
codes in your claim statement for more details.
Benefit exclusions
Benefit exclusions can be:
- Any billed services that are not covered by your plan
- Costs you may have to pay if you use an out-of-network provider
You will not be charged when an exclusion is due to
billing errors or missing information needed to complete a claim. Those
exclusions are the doctor’s responsibility and will not be added to the
amount you pay.
Please check the reason codes in your SmartSummary Explanation of Benefits (EOB) for more details.
Amount Humana paid
The amount your Humana plan pays toward your claim(s).
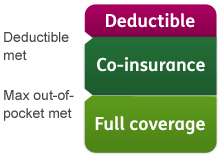
Maximum out-of-pocket
The most money you will be required to pay for covered
medical services and prescription drugs in a calendar year. This amount
includes copayments, deductibles and coinsurance.
Plan paid
The amount your plan paid toward your claim(s).
Part B
Medicare medical insurance helps pay for doctors' services, outpatient
hospital care, durable medical equipment and some medical services not
covered by Part A. This claim was processed under the Part B benefit.
Part D
This claim was processed under the Part D benefit. Part D covers
prescription drug coverages through Medicare-approved prescription drug
plans offered by private companies. Part D plans are available to anyone
eligible for Medicare benefits under Part A or enrolled in Part B.
DDW (Drug Discount Wrap)
This program assists Humana members when they need to buy drugs that are
not a covered benefit. This claim was processed as a DDW.
Centers for Medicare and Medicaid Services (CMS) excluded
This claim type covers medicines that are excluded by Medicare (CMS), but may or may not be covered under a plan benefit.
DMR (Direct Member Reimbursement)
DMR is used to reimburse Humana members. This occurs when a member paid
out of pocket in place of using their insurance. This claim processed
under DMR.
OTC (Over the Counter)
These are medicines sold directly to a consumer. They do not need a
prescription from a healthcare professional. This drug was processed as
an OTC drug.
PA (Prior Authorization)
There are certain drugs Humana must approve before your plan will cover
them. This claim was processed with a prior authorization number.